Joint pain and osteoarthritis: Management

Managing joint pain and osteoarthritis
Joint pain can impinge on all areas of a person’s life, particularly in older individuals.
Together with education, a range of pharmacological and non-pharmacological techniques is available to help manage pain and flare-ups1,2 and help keep patients moving.
Guideline recommendations for treating joint pain and osteoarthritis
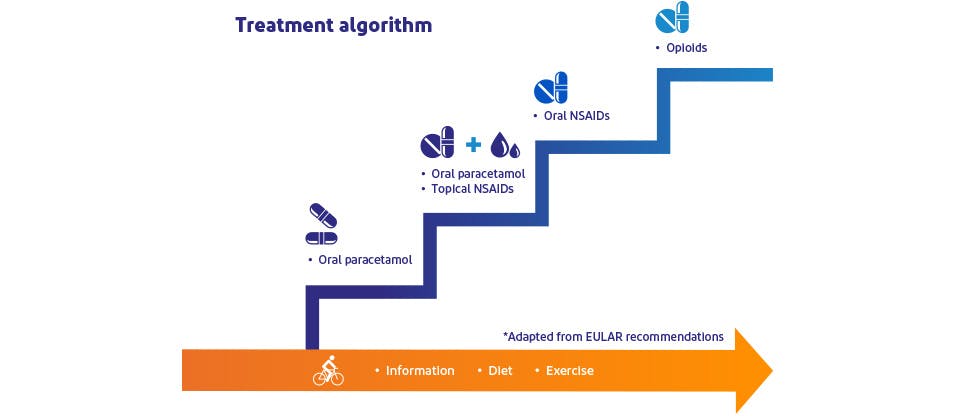
Guidelines recommend a stepped approach to management2,4–6
Management of osteoarthritis may require a combination of non-pharmacological and pharmacological modalities.2,6
Guidelines* recommend a stepwise strategy for the pharmacological management of osteoarthritis.2,4–6
*From the National Institute for Health and Care Excellence (NICE), European League Against Rheumatism (EULAR) and American College of Rheumatology (ACR).
More than one pain treatment might be needed

Additional support might be needed to cover pain flares
Chronic joint pain is often accompanied by acute inflammatory flares.7
During this flare-up pain, patients may require additional short-term pain relief.7
How can Nora be helped?

Nora
Nora wakes with joint pain and stiffness each morning.
She wants sustained relief from her pain so she can return to the activities she enjoys, like walking and spending time with her grandchildren. However, she is concerned about treatment side effects.
Nora needs to regain her mobility by easing joint pain.
PANADOL Joint delivers effective pain relief of chronic joint pain for up to 8 hours.22 Paracetamol is one of the most used analgesic and antipyretic over-the-counter drugs.23
Voltaren Emulgel 12 Hours combats flare-up pain from osteoarthritis,24–26 and provides up to 12 hours of relief from joint pain in a convenient, twice-daily topical treatment. Topical diclofenac has a low systemic absorption, meaning a lower risk of systemic side effects.25
Understanding joint pain and osteoarthritis
Signs and symptoms
Explore an overview of how to recognise joint pain and osteoarthritis and know when to refer patients.
Overview of sprains and strains
Find out about how common sprains and strains are, and meet two patients with these problems.
Learn more
Voltaren Emulgel 12 Hours for joint pain and osteoarthritis
Up to 12 hours of relief from joint pain.24

Back pain management
Learn how superficial heat fits into the overall management approach to back pain.